One of the biggest ironies about having IBS is that, often, eating a plant-based diet or ‘healthy food’ can actually make you feel worse. Why? Plant-based diets are often high in fibre – and while fibre is good for gut health, certain elements of fibre can trigger uncomfortable IBS symptoms.
BUT if you can tolerate a slow increase in plant-based foods, it will mean an increase in ‘good’ bacteria in your gut. All you need to understand is which foods work well for you (and which don’t).
Confused about where to start? We caught up with two gut health specialists to find out what is IBS, how best to manage it and whether eating a plant-based diet can really help…
Meet the experts: Clarissa Lenherr, registered nutritionist and gut health specialist. Priya Tew, specialist Dietitian from Dietitian UK and author of The Complete Low FODMAP diet plan.
What is IBS?
‘IBS – or irritable bowel syndrome – is a common condition that affects the digestive system and can cause a variety of symptoms such as abdominal pain, bloating, constipation, and diarrhoea,’ explains Clarissa Lenherr, registered nutritionist and gut health specialist.
‘IBS is a functional gut disorder,’ adds Priya Tew, specialist Dietitian from Dietitian UK and author of The Complete Low FODMAP diet plan. ‘This is where your digestive system is not working as it should but tests do not show signs of inflammation, physical damage or abnormalities. There are 3 types of IBS: IBS-C (constipation), IBS-D (diarrhoea) and IBS-M (a mix of the 2).’
The exact cause of IBS is unknown, but several factors that may contribute to its development, include:
-
Abnormalities in gut muscle contractions
-
Abnormalities in an individual’s gut bacteria
-
Increased sensitivity to pain in the gut
-
Psychological stress
-
Food intolerances or sensitivities
-
Hormonal changes in women
-
A previous gastrointestinal infection
-
Dysbiosis – an imbalance of bacteria in the gut
-
SIBO – small intestinal bacterial overgrowth
Is there a specific test to diagnose IBS?
Unfortunately, there isn’t a specific test to diagnose IBS, says Lenherr – since ‘it’s primarily diagnosed based on symptoms and by ruling out other conditions. Doctors may conduct several tests to rule out other potential causes of symptoms that mimic IBS such as checking for Coeliac disease and IBD.’
There are no clinical markers to test using blood tests and nothing that shows up as abnormal in investigations – ‘even if you look inside the gut,’ adds Tew.
Are there certain factors that increase your risk of getting IBS?
‘Some people develop IBS symptoms following an infection such as gastroenteritis or food poisoning,’ says Lenherr. ‘This is known as post-infectious IBS (PI-IBS), and it’s thought to result from changes in the gut microbiota and immune system function.
‘Women are also more likely to get IBS than men,’ she adds.
Tew says a family history of IBS can predispose you, and hormonal changes and high-stress levels can affect IBS symptoms. ‘We saw a lot more IBS due to the pandemic for example,’ she says.
How is IBS managed?

Diet
Diet is arguably one of the most important strategies when it comes to dealing with IBS. ‘Many people with IBS find that certain foods/drinks can trigger or worsen their symptoms,’ says Lenherr. ‘These can include gas-producing foods like beans and broccoli, high-fat foods, caffeine, alcohol, spicy foods, artificial sweeteners, and gluten-containing foods.’
Her advice? ‘Aim to eat three regular, well-balanced meals a day with one snack if needed between lunch and dinner. Avoid grazing (constantly snacking) and try to leave 3-4 hour gaps between meals and snacks to allow your MMC (migrating motor complex) to do its job at clearing out the digestive system.’
Tew agrees, and suggests opting for small frequent meals instead of larger meals. ‘Chew food well and take your time over meals,’ she adds, ‘eat away from work and distractions like the TV so you connect with your food in a calm environment where possible.’
Staying hydrated also really helps as hydration levels can have a big impact on bowel function and motility. Lenherr reminds us to drink at least 2 litres of filtered water per day.

Stress management
Whilst diet can play a key role it is not the only strategy in managing IBS, says Tew. ‘There is a huge link between the gut and the brain, often called the gut-brain pathway. This means if the brain is stressed then the gut can also be stressed and vice versa. Which is why IBS symptoms can be worse in times of stress.
‘Now we may not be able to remove the stress but we can work on how we deal with stress. So working on calming your nervous system can really help using strategies like mindfulness, meditation, calming activities, yoga and gut-related hypnotherapy.’

Mindful eating
‘Eating slowly and mindfully, including taking the time to chew food thoroughly, can help people become more attuned to their body’s signals of hunger and fullness,’ says Lenherr. ‘It can also help reduce stress and anxiety around meal times, which are common triggers for symptoms in some people with IBS.’
FODMAP diet
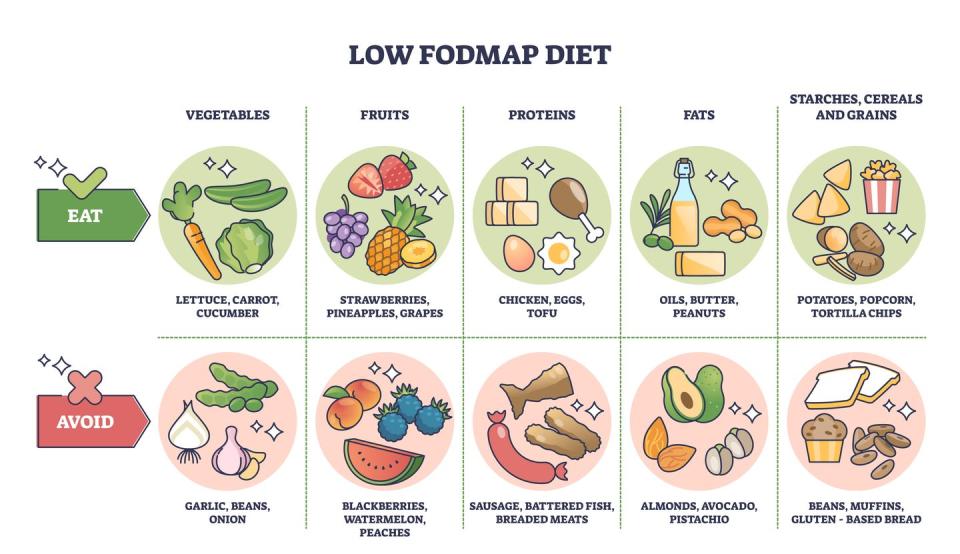
The low FODMAP diet has been found to reduce IBS symptoms in up to 70% of those with IBS.
What are FODMAPS?
‘FODMAPS are fermentable, poorly absorbed, short-chain carbohydrates found in everything from bread to garlic, and even some fruit like apples and pears,’ explains Lenherr. ‘For some, eating fodmap-containing foods may trigger symptoms such as bloating, gas, stomach pain, diarrhoea and constipation.’
The acronym ‘FODMAP’ stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols.
Tew breaks down the science:
-
Oligosaccharides: These include fructans and galacto-oligosaccharides (GOS). They’re found in foods like wheat, onions, garlic, legumes (like beans and lentils), and certain fruits and vegetables (like asparagus and artichokes.)
-
Disaccharides: The main culprit here is lactose, which is found in dairy products like milk, yoghurt, and soft cheeses.
-
Monosaccharides: This refers to excess fructose, which is found in some fruits (like apples, pears, and watermelons) and honey.
-
Polyols: These are sugar alcohols found naturally in some fruits and vegetables (like avocado, cherries, and cauliflower), as well as in some artificial sweeteners (like sorbitol, mannitol, and xylitol).
How do you follow a FODMAP diet?
-
Elimination phase – eliminate high FODMAP foods from your diet for 2- 6 weeks.
-
Reintroduction phase – gradually reintroduce FODMAP-containing foods one at a time, in gradually increasing portions, to identify your specific trigger foods and the portions you can tolerate.
-
Personalise – figure out a diet that involves limiting your trigger foods but avoiding nutritional deficiencies.
Foods high in FODMAPS:
-
Dairy-based milk, yoghurt and ice cream
-
Wheat-based products such as cereal, bread and crackers
-
Some vegetables, such as garlic, onions and mushrooms
-
Some fruits, such as apples, cherries, pears, watermelon and peaches
Foods low in FODMAPS:
-
Eggs and meat
-
Grains like rice, quinoa and oats
-
Nuts and seeds
-
Vegetables like potatoes, tomatoes, cucumbers and courgettes
REMEMBER: It’s important to follow the low-fodmap diet alongside a nutritionist or dietitian trained in the low-fodmap approach, as the diet is very restrictive and, if followed long-term, may increase your risk of nutritional deficiencies.
Plant-based IBS diet
Eating a plant-based diet has lots of health benefits, but experts remain unconvinced as to whether it has any specific benefits for IBS sufferers in particular.
‘Eating a well-balanced, plant-based diet filled with veggies, pulses, nuts and seeds might help some people with IBS – especially if they were lacking in fibre and this was leading to constipation. However, lots of plant-based diets are filled with ultra-processed foods and ingredients that might trigger digestive upset,’ says Lenherr.
‘In addition, lots of plant-based foods are filled with FODMAPS, which we know can trigger some people who have IBS.’
So, while it’s totally possible to stick to a plant-based diet if you have IBS, it can be a challenge. ‘It just requires more planning in order to make sure you meet your nutritional needs,’ says Tew.
A plant-based diet, if well-balanced, can provide ample nutrients, however, it requires careful consideration to ensure you’re getting all essential nutrients, particularly vitamin B12, iron, calcium, omega-3 fatty acids, and protein. As the low fodmap diet restricts portion sizing of many pulses and tofu, it can be a challenge to get in good amounts of plant-based protein.
The bottom line: Any form of dietary restriction will make it more difficult for you to meet all your nutritional requirements. As always, if you suspect that you have IBS, reach out to health professional to ensure you have a proper diagnosis and ask for a referral to a dietitian for advice on dietary options to help manage your symptoms.
Cut through the noise and get practical, expert advice, home workouts, easy nutrition and more direct to your inbox. Sign up to the WOMEN’S HEALTH NEWSLETTER
More in Nutrition
You Might Also Like
Source: bing.com




















